What You Need to Understand Medicaid

"All people, including people with intellectual and/or developmental disabilities (I/DD), should have timely access to high quality, comprehensive, accessible, affordable, appropriate health care that meets their individual needs, maximizes health, well-being and function, and increases independence and community participation."
To read more of The Arc’s Position Statement on Health Care, click here.
Medicaid
Provides health coverage to millions of Americans, including eligible low-income adults, children, pregnant women, elderly adults and people with disabilities. Medicaid is administered by states, according to federal requirements. The program is funded jointly by states and the federal government.
NJ FamilyCare is New Jersey's Medicaid program that provides public health care coverage throughout the state.
There are two primary programs:
- NJ FamilyCare, covering children under 19, adults, and pregnant women.
- NJ FamilyCare Aged, Blind, Disabled (ABD) Programs, covering people 65 and older, and people determined blind or disabled by the Social Security Administration (SSA) or State of NJ. The majority of individuals with IDD receive Medicaid through the ABD programs.
The NJ FamilyCare ABD Programs include:
- Supplemental Security Income (SSI) Medicaid
- Medicaid Only
- New Jersey Care... Special Medicaid Programs
- NJ WorkAbility
- Long Term Services and Supports (LTSS)
Some individuals with IDD who receive SSI and Medicaid subsequently lose both upon the retirement, disability, or death of a parent. This occurs because the individual with IDD starts receiving a Social Security benefit, or Survivor's benefit, via the parent that results in them being ineligible for SSI. In this instance, however, they can still qualify for Medicaid as a Disabled Adult Child (DAC) under Section 1634 of the Social Security Act.
Other individuals with IDD may not have been on SSI or Medicaid before they began receiving Social Security from the retirement, disability, or death of a parent, often preventing them from applying for SSI Medicaid. Individuals with IDD making less than 100% of the Federal Poverty Level (FPL) or $1,255/month (2024) can apply for Special Medicaid through their local County Board of Social Services. If the individual is making more than 138% of the FPL or $1,732/month (2024), can apply for special status through DDD whereby the individual completes a DDD intake application and, upon approval for services, would receive a Medicaid application through the DDD waiver unit when approaching age 21.
Certain individuals with IDD become eligible to receive Medicare, in addition to Medicaid, before the age of 65. These individuals are referred to as "Dual Eligibles." For example, this often occurs when an individual with IDD receives a Social Security benefit off a retired parent's work record for 24 months, after which the individual automatically starts to receive Medicare.
Medicaid is a requirement to receive services from the New Jersey Division of Developmental Disabilities (DDD), which become available once an individual with IDD turns 21. For more information and a list of additional Medicaid resources, visit DDD’s website.
DDD administers two Medicaid waiver programs, the Supports Program and Community Care Program (CCP). They are intended to provide individuals with home and community based supports based on their personal needs and budget.
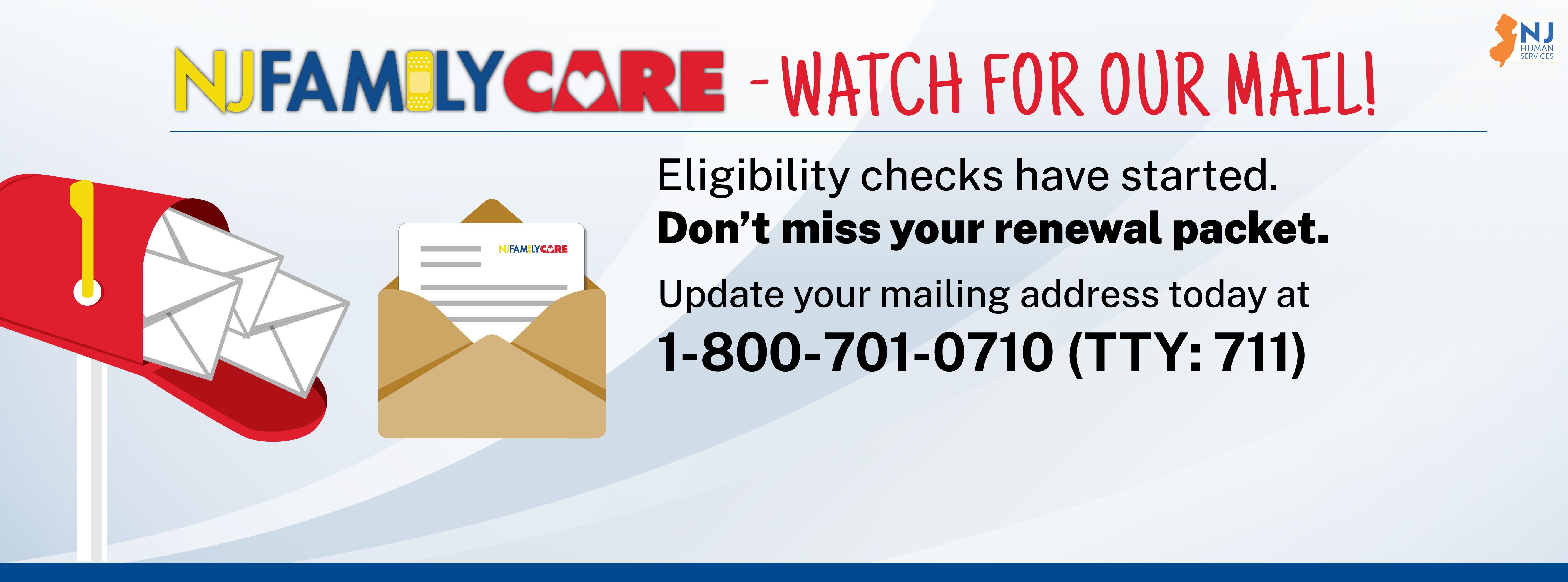
Medicaid Unwinding
From March 2020 to March 2023, NJ FamilyCare/Medicaid followed special rules related to the federal COVID-19 Public Health Emergency (PHE). These rules allowed NJ FamilyCare/Medicaid members to keep their health coverage, even if they no longer qualified.
However, Congress passed legislation that requires state Medicaid programs to go back to the rules that were used prior to the start of the COVID pandemic. This process, which is known as "Medicaid Unwinding," will last for 12 months. Therefore, each month, since April 1, 2023, 1/12th of the NJ FamilyCare/Medicaid beneficiaries will receive a Medicaid redetermination application. The exception to the requirement of completing a Medicaid redetermination application is individuals with IDD who receive Supplemental Security Income (SSI).
As part of this review, many members will receive mail from the State of New Jersey or their County Board of Social Services. Members will have to provide or confirm additional information so NJ FamilyCare/Medicaid can decide whether they still qualify for healthcare coverage. Members who do not respond to NJ FamilyCare/Medicaid mail may lose their coverage.
Health Care Advocacy
The Arc of New Jersey's Health Care Advocacy Program promotes quality health care for people with intellectual and developmental disabilities throughout New Jersey.
If you are having difficulties with Medicaid, please feel free to submit a problem form, found here.
The program also offers numerous other resources related to Medicaid Unwinding and Medicaid.
Medical Assistance Customer Centers (MACCs)
Available to provide customer service to NJ FamilyCare members and the public. Contact your local county MACC office.
Other Links and Resources
- NJ FamilyCare/Medicaid
- Medicaid ABD Programs
- Different Types of NJ Medicaid Fact Sheet
- Eligibility for ACA expansion Medicaid
- NJ WorkAbility Medicaid Fact Sheet
- Apply online for Medicaid
- Division of Medical Assistance and Health Services (DMAHS)
- NJ Medicaid Managed Care Organizations (MCOs)
- The Arc of NJ Health Care Advocacy Medicaid Resources
- NJ Medicaid and Private Health Insurance Fact Sheet
- Split Application Medicaid Fact Sheet
- Dual Eligible Individuals with Medicare and Medicaid FAQs
- Dual Eligibles and Prescription Medication FAQs
- Dual Eligibles and Special Needs Plans (D-SNPs) FAQs
- Division of Developmental Disabilities (DDD) and Medicaid Eligibility
- NJ FamilyCare Personal Care Assistant (PCA) Services
- NJ FamilyCare Personal Preference Program (PPP)